Keratoconus Treatment in Flower Mound
Looking for expert keratoconus treatment in Flower Mound, Texas? PersonalEyes Vision Care provides specialized keratoconus care with advanced corneal topography and custom contact lens fitting. Dr. Kumar Patel, a board-certified optometrist with specialty lens expertise, offers comprehensive keratoconus management including scleral lenses and corneal cross-linking coordination.
Keratoconus is a progressive eye condition that affects the cornea's shape, causing vision distortion that glasses often cannot correct. Early detection and proper treatment are crucial for maintaining clear vision and preventing progression. Our Flower Mound practice serves patients throughout the DFW area with personalized keratoconus care plans and the latest treatment technologies.
Expert Keratoconus Care with Dr. Kumar Patel
Dr. Kumar Patel provides top-tier keratoconus treatment in Flower Mound. He thoroughly educates patients about their eye conditions and presents the most up-to-date treatment options available.
As a Board Certified Optometrist, Dr. Patel specializes in custom specialty contact lenses used to manage various eye conditions including keratoconus, pellucid marginal degeneration, post-RK complications, and severe dry eyes. Learn more about our comprehensive eye care services.
Specialty Expertise: Dr. Patel's advanced training in specialty contact lens fitting makes PersonalEyes Vision Care a leader in keratoconus management in the DFW area.
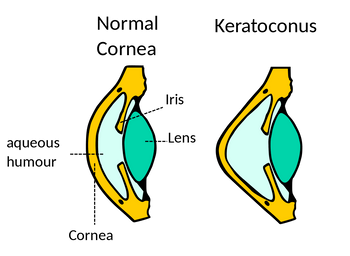
What is Keratoconus?
Keratoconus is a progressive eye condition where the cornea (the clear front surface of your eye) gradually thins and bulges into a cone-like shape. This irregular shape distorts vision, often making it impossible to achieve clear sight with regular glasses or soft contact lenses.
The condition typically begins during teenage years or early twenties and can progress for 10-20 years before stabilizing. Early detection and proper management are crucial for maintaining good vision and quality of life.
Learn More: For additional information about keratoconus, visit the American Academy of Ophthalmology.
Keratoconus Causes and Risk Factors
While the exact cause of keratoconus remains unknown, researchers have identified several risk factors that may contribute to its development. Understanding these factors can help with early detection and prevention strategies.
Possible Contributing Factors
- Genetics: Family history increases risk significantly
- Eye rubbing: Chronic rubbing due to allergies or irritation
- Collagen abnormalities: Weakened corneal tissue structure
- UV exposure: Excessive ultraviolet light exposure
- Hormonal changes: Particularly during puberty and pregnancy
Associated Conditions
- Down syndrome
- Ehlers-Danlos syndrome
- Marfan syndrome
- Retinitis pigmentosa
- Atopic dermatitis (eczema)
Keratoconus Symptoms
Keratoconus typically develops gradually, with symptoms becoming more noticeable as the condition progresses. The disease usually affects both eyes, though one eye may be more severely affected than the other.
Early Symptoms
- Blurred or distorted vision
- Increased light sensitivity
- Frequent prescription changes
- Difficulty with night vision
Advanced Symptoms
- Severe vision distortion
- Multiple ghost images
- Halos around lights
- Contact lens intolerance
Important: Early detection is crucial. If you experience frequent prescription changes or progressive vision distortion, schedule a comprehensive eye exam with Dr. Patel immediately.
Advanced Keratoconus Diagnosis
At PersonalEyes Vision Care, we use state-of-the-art diagnostic technology to detect keratoconus in its earliest stages. Our advanced corneal topography system can identify even subtle corneal changes before symptoms become apparent.
Our TopCon CA-800 Corneal Topographer Features:
- Built-in Keratoconus Screening: Automated detection algorithms for reliable diagnosis
- Corneal Elevation Maps: Detailed 3D mapping of corneal shape irregularities
- Pachymetry Measurements: Precise corneal thickness monitoring
- Progression Tracking: Compares current scans with baseline measurements
- Contact Lens Fitting Data: Provides measurements for specialty lens design
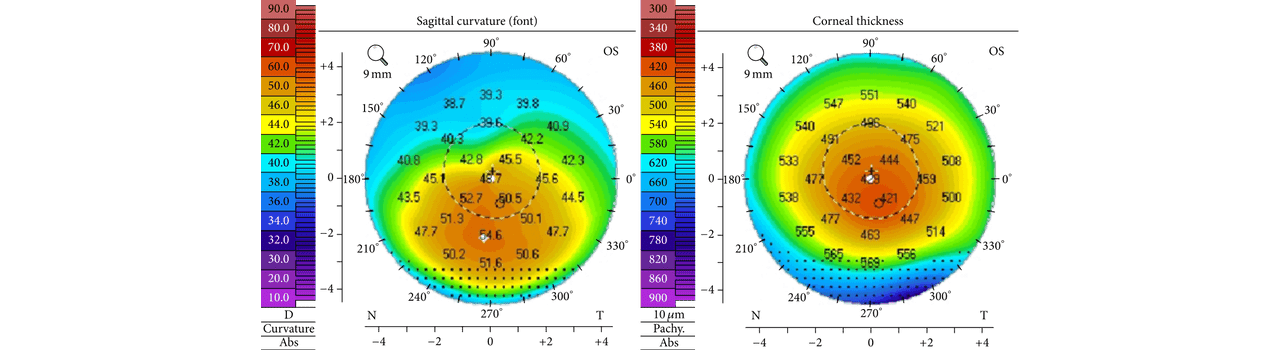
The left scan shows characteristic inferior steepening (hallmark of keratoconus). The right scan reveals central corneal thinning (400 microns vs. normal 500+ microns).
Comprehensive Keratoconus Treatment Options
Treatment for keratoconus depends on the severity and progression of the condition. Dr. Patel creates personalized treatment plans that may evolve as your condition changes over time.
Early Stage Treatment
- Prescription glasses
- Soft toric contact lenses
- Regular monitoring
- UV protection
Moderate Stage Treatment
- Rigid gas permeable (RGP) lenses
- Hybrid contact lenses
- Custom soft lenses
- Corneal cross-linking evaluation
Advanced Stage Treatment
- Scleral lenses (gold standard)
- Piggyback lens systems
- Surgical consultation
- Corneal transplant evaluation
Gold Standard Care: Scleral lenses are now considered the gold standard for keratoconus treatment, providing excellent vision correction and corneal protection. Learn more at the National Keratoconus Foundation.
Corneal Cross-Linking (CXL)
For patients with progressive keratoconus, corneal cross-linking represents a breakthrough treatment option. This FDA-approved procedure can halt or slow the progression of keratoconus, potentially preventing the need for corneal transplant surgery.
How CXL Works
- Riboflavin (vitamin B2) drops are applied to the cornea
- Controlled UV-A light activates the riboflavin
- New collagen cross-links form, strengthening the cornea
- Corneal bulging is halted or significantly slowed
Benefits of CXL
- Stops or slows keratoconus progression
- May improve corneal shape
- Preserves existing vision
- Outpatient procedure with quick recovery
CXL Coordination: While PersonalEyes Vision Care doesn't perform CXL procedures, Dr. Patel works closely with corneal specialists to determine candidacy and coordinate treatment when appropriate.
Expert Keratoconus Care in Flower Mound
Don't let keratoconus compromise your vision. Schedule a comprehensive evaluation with Dr. Kumar Patel to explore your treatment options and preserve your sight.
Frequently Asked Questions About Keratoconus
At what age does keratoconus typically develop?
Keratoconus usually begins during the teenage years or early twenties. It can progress for 10-20 years before stabilizing. Early detection through regular eye exams is crucial for optimal management.
Can keratoconus be cured?
While there's no cure for keratoconus, it can be effectively managed with proper treatment. Corneal cross-linking can halt progression, and specialty contact lenses provide excellent vision correction for most patients.
How successful are scleral lenses for keratoconus?
Scleral lenses are highly successful for keratoconus patients, with success rates over 90%. They provide excellent vision correction, all-day comfort, and protection for the irregular corneal surface.
Is keratoconus hereditary?
Yes, keratoconus has a genetic component. If you have a family history of keratoconus, you're at higher risk and should have regular comprehensive eye exams for early detection.
Learn more about our comprehensive eye care services or read about Dr. Kumar Patel's specialty lens expertise. Share this page to spread awareness about keratoconus care!
Reading time: 6 minutes
Last updated: May 27, 2025
