Dr. Kumar Patel believes in educating his patients thoroughly about their eye conditions and presenting any treatment options currently available. As a Board Certified Optometrist, he specializes in custom specialty contact lenses that are used to manage various eye conditions including Keratoconus, Pellucid Marginal Degeneration, Post RK, and Severe Dry Eyes. Let’s dive into what Keratoconus actually is.
What is Keratoconus?
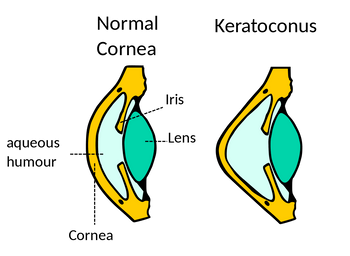
Keratoconus is an extremely slow moving eye condition which entails progressive thinning of the front part of the eye, called cornea, into a cone shape. The cornea is the clear, dome shaped tissue that covers the colored part of the eye (iris). In those patients with Keratoconus, the now cone-shaped cornea deflects light and causes distorted vision uncorrectable by glasses.
What causes Keratoconus?
The year is 2020 and there still is no definitive cause of Keratoconus. Possible causes include:
- Genetics
- Excessive eye-rubbing (i.e allergies)
- Collagen deficiency
- Overexposure to ultraviolet rays from the sun
Symptoms of Keratoconus
Keratoconus can develop at any age, but the beginning stages of reshaping may start in the teen years to the early 20s. Changes in the shape of the cornea occur over several years. In most patients with Keratoconus, both eyes eventually become affected. Constant distorted vision and night time glare still present with the most updated glasses may be the first signs of Keratoconus. Other signs include increasing myopia and astigmatism every year.
How do I know if I have Keratoconus?
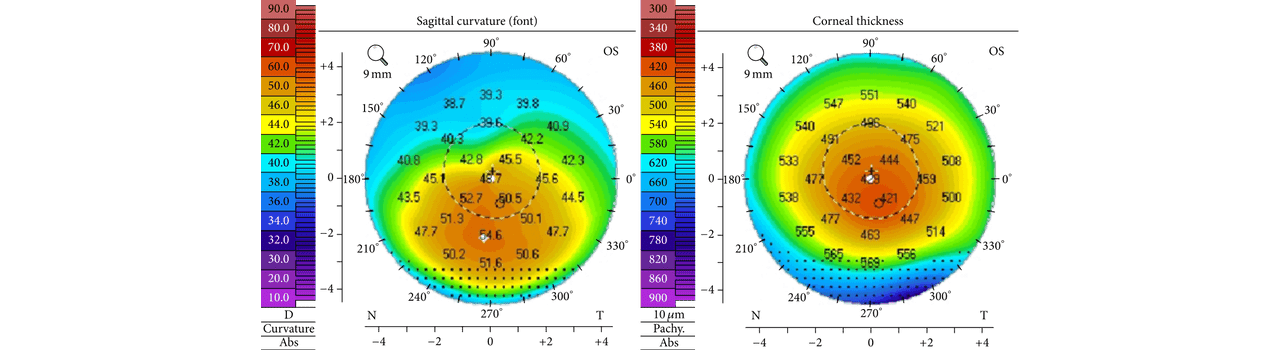
Optometrists are the first in line to diagnose Keratoconus. This is done by evaluating the cornea thoroughly. Gold standard method includes analysis via corneal topographer (Click here to read about our TopCon CA-800 Corneal Topographer. This instrument can detect the smallest corneal change and record it for future comparisons. At PersonalEyes, our corneal topographer has a built in Keratoconus Screening tool which helps make our diagnosis more reliable. Viewing the example below, the left scan shows steepening on the lower 1/3rd of the cornea (hallmark sign of Keratoconus). On the right scan, you can see the central corneal thinner than the peripheral corneal (low 400 microns vs mid-500 microns).
Secondly, doctors view the cornea thru a microscope and evaluate the presence of corneal thinning or irregularities indicative of Keratoconus.

How do you treat Keratoconus?
In early stages, regular glasses and soft contact lenses sufficient to treat Keratoconus. If patients are not able to achieve acceptable vision with glasses or soft contact lenses, other options are available. In these cases, specialty lenses are used to provide more clear and comfortable vision. These lenses include Rigid Gas Permeable lenses, Scleral Lenses, and Hybrid lenses. In advanced cases, a corneal transplant may be necessary.
Is there a surgical option?
If diagnosed early and proof of progression in your cornea is observed, a special procedure called Corneal Cross Linking can be done to help prevent the worsening of this condition. Collagen Cross-Linking is a relatively new method (Approved in the US in April 2016). It works by strengthening the corneal tissue to stop it from becoming more cone shaped or bulging. In this procedure, eye drops containing riboflavin (vitamin B2) are applied to the cornea and then activated by ultraviolet light. This strengthens the collagen fibers within the cornea and prevents the worsening of this condition.
